Reflecting on this year's National Academy for State Health Policy’s (NASHP) State Health Policy Conference in Jacksonville, Florida, I am amazed by all the recent healthcare innovations, which are resulting in policies with real and positive effects on health outcomes.
Why innovate?
A panel discussion during the August 16, 2018, Morning Plenary focused on making average citizens aware of the healthcare issues related to cost and outcomes—and how to drive home the impact of these issues. The panel suggested that the average citizen should be aware that:
- Healthcare costs in the United States are twice as much as healthcare costs in peer countries.
- Despite this difference in healthcare costs, healthcare outcomes in the United States are about the same or worse than healthcare outcomes in peer countries.
- Ultimately, people in the United States don’t use more healthcare than people in peer countries—yet they pay significantly more.
One panelist pointed out that the amount of money an average U.S. family of four spends on healthcare per year is comparable to the cost of a new car. Often, families just don't know the full healthcare costs because employers pay portions.
All of these points are good reminders that healthcare can be a great source of innovation when consumers have more information to make decisions, and that policy makers are figuring out ways to address the social determinants of health.
Examples of innovation
During the breakout sessions that I attended at the conference, I thought about the amazing progress that states are making in addressing social determinants of health and the transparency of healthcare costs. Then, during the “Innovations in Rural Health Policy Options” session, Nitika Moibi from the Minnesota Department of Health reminded us of the Innovation Adoption Curve. The Innovation Adoption Curve is a model that helps us understand the adoption of new ideas from innovation through market saturation.
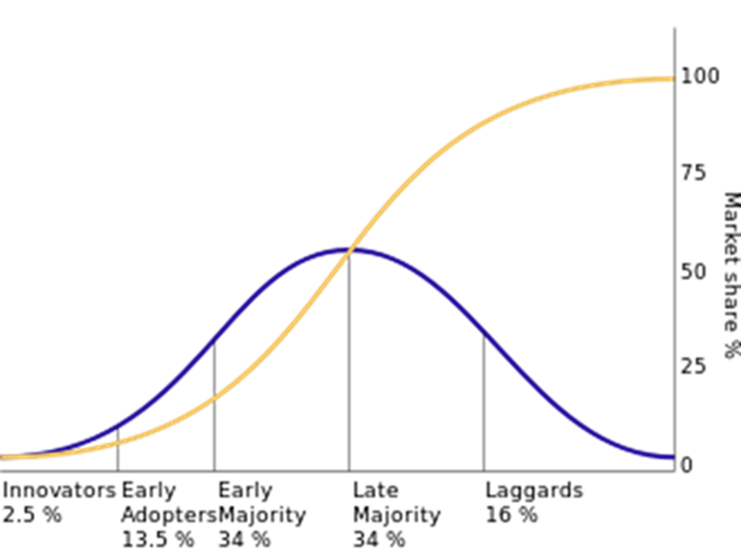
Blue line: Consumers adopting new technology
Yellow line: Market share of the technology
Source: https://en.wikipedia.org/wiki/Diffusion_of_innovations
The discussion of the Innovation Adoption Curve reminded me of the fact that health policy is driving innovation—which may help address healthcare costs and improve outcomes. Some examples of this innovation discussed during the various breakout sessions I attended include:
- Second Harvest Heartland, a Minnesota foodbank, works with clinics to help people with food insecurity. This, in turn, is leading to improved dietary adherence and outcomes for diabetic patients.
- Utah is now sharing cost information, which improves the efficiency of the market by allowing consumers to make informed decisions. One benefit of this is growing awareness that options for certain procedures are cheaper when conducted in a provider’s office than in an outpatient center or a hospital. Utah State Senator Daniel Hemmert further explained that in addition to this cost information, Utah provides an assessment of quality and cost, along with alerts to inform consumers of potential additional costs, such as higher cost lab or pharmacy practices.
- Paula Kaiser VanDam, Michigan’s Director of the Bureau Community Services, talked about the state’s Community Health Innovation Region (CHIR) program, which is operated through Michigan’s State Innovation Model (SIM) grant. By screening people for social determinants of health, the program brings together health services and social services. Michigan is also persuading healthcare workers to think about social determinants of health beyond those with immediate clinical impact. For example, when organizing transportation to take a patient to a clinic, healthcare workers should also organize transportation to take the patient to food sources. That way, the patient can secure their next meal.
There were many additional great examples of innovative health policy, such as Georgia's tele-health program and Rhode Island's social determinants of health. Based on what I heard during the breakout sessions, many states would fall into either the “Innovators” or “Early Adopters” categories on the Innovation Adoption Curve.
Up next
All of this innovation is very exciting. And I think there is room for more excitement. Consider the opportunities for improving long-term health outcomes for children. After hearing about the great work that is being done by Second Harvest Heartland, I asked one Medicaid director about similar programs for children, and we had a great discussion. Right now, it appears that programs specifically targeting children are limited. This is because children typically cost the healthcare system less than the adults being targeted for interventions.
However, during my conversation with the Medicaid director, there was agreement that low-cost children turn into expensive adults, and interventions can turn those children into productive adults, which grows the future economy and saves states money that can be repurposed or given back to taxpayers. Opportunities include leveraging doulas to screen expectant mothers for their social determinants of health in an effort to help prevent Adverse Childhood Experiences (ACEs) for their unborn children. These opportunities may translate into action, with states leveraging 1115 waivers and the Integrated Care for Kids model to drive further innovation. The 1115 waiver approach is similar to what our friends in Hawai‘i are driving toward with their Hawai‘i Ohana Nui Project Expansion (HOPE), which seeks to improve health outcomes through a multi-generation approach to addressing public health needs.
Please continue the conversation with me or find me next year at the NASHP Conference in Chicago.